Endometriosis and Fertility: A Closer Look at Unexpected Conception Benefits
The topic of endometriosis and its effect on fertility is full of tricky parts that often leave patients and clinicians alike working through a maze of confusing bits. Recent research suggests that women diagnosed with endometriosis might experience a surprising advantage when it comes to conceiving compared to those with other infertility causes. While the subject is loaded with challenging issues, a closer look at the evidence and the many subtle details can provide hope and clarity for those affected by this condition.
Over the past few decades, the medical community has observed that endometriosis—a condition where tissue resembling the uterine lining grows outside the uterus—affects millions of women worldwide. Many assume that this condition always makes the journey to pregnancy more nerve-racking. However, emerging studies indicate that the reality might be more nuanced, with some findings suggesting that conception rates can be unexpectedly higher in women with endometriosis than in those with other causes of infertility.
Understanding Endometriosis: The Fine Points of a Complicated Condition
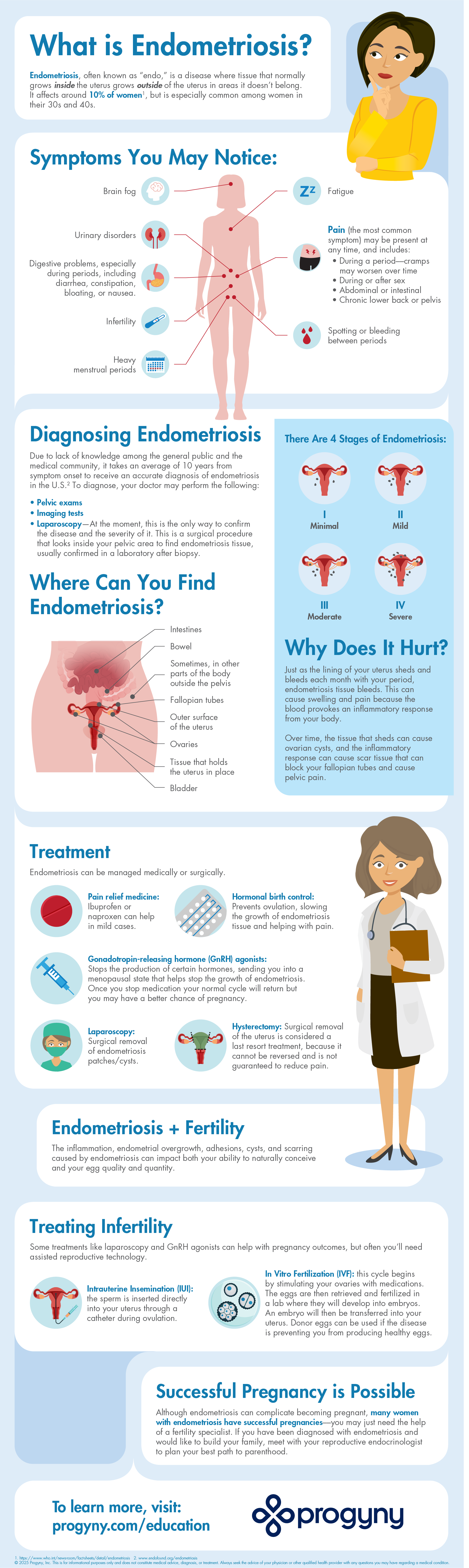
Endometriosis is notorious for its tangled issues and intense symptoms, which can include chronic pelvic pain, heavy menstrual bleeding, nausea, fatigue, and even emotional challenges such as depression or anxiety. It is also known to interfere with fertility, making this topic both essential and complicated in planning for a family.
Defining the Condition and Its Impact on Quality of Life
To get into the subject, it is important to define what endometriosis is and how it affects day-to-day life. The condition occurs when tissue similar to the endometrium (the lining of the uterus) grows outside the uterus, often on the ovaries, fallopian tubes, and other structures within the pelvis. This misplaced tissue behaves much like the lining of the uterus—it thickens, breaks down, and bleeds with each menstrual cycle, which can lead to inflammation and scar tissue formation.
The symptoms of endometriosis have been described in various ways, from the common and understandable signs of heavy bleeding and pelvic pain to the more complicated pieces such as persistent fatigue and emotional stress. Patients often experience delays in receiving a diagnosis because the twists and turns of identifying the condition require a careful evaluation that might include imaging studies, physical examinations, and even surgical interventions such as laparoscopy. Early diagnosis and management of endometriosis are considered essential to addressing the condition and improving a patient’s overall quality of life.
How Endometriosis Can Influence Fertility
When it comes to fertility, many patients and healthcare providers assume that endometriosis is a barrier to conception. However, recent data suggests an intriguing twist—women with endometriosis have been reported to have conception rates that are up to four times higher than women facing infertility due to other causes. This counterintuitive outcome may be partly due to increased vigilance on the part of patients and the timeliness of seeking fertility treatments after an early diagnosis.
A key theory is that heightened awareness about endometriosis prompts women to seek specialized fertility care sooner. Early diagnosis can often lead to timely interventions, such as laparoscopic surgery, which might not only manage the condition’s symptoms but also improve the reproductive potential by addressing adhesions and other physical issues that can interfere with natural conception.
Diagnostic Challenges: Unraveling the Twists and Turns of Detecting Endometriosis
One of the most intimidating aspects of dealing with endometriosis is the challenge of obtaining an accurate and timely diagnosis. It is not uncommon for patients to feel overwhelmed by the process. The journey to a definitive diagnosis is riddled with issues that range from confusing symptom presentations to the need for invasive procedures to confirm the diagnosis.
Identifying the Subtle Signs in the Early Stages
In many cases, the early signs of endometriosis may be dismissed as normal menstrual discomfort rather than indicators of an underlying condition. Patients might experience subtle details regarding pelvic discomfort or irregular bleeding that are easily mistaken for typical cycle-related issues. However, consistent or severe symptoms should prompt a deeper evaluation, ideally before the condition advances to create more complicated pieces such as extensive scarring or significant anatomical distortion.
The following table outlines some key indicators often associated with early endometriosis:
| Symptom | Description |
|---|---|
| Pelvic Pain | Chronic pain that can worsen during menstruation |
| Heavy Menstrual Bleeding | Excessive bleeding that goes beyond a normal flow |
| Fatigue | A persistent sense of tiredness, sometimes accompanied by malaise |
| Nausea | Gastrointestinal upset during menstrual cycles |
| Emotional Stress | Mood disturbances including anxiety and depression |
This list is not exhaustive, but it represents some of the common signs that should encourage an individual to seek medical advice. Recognizing these subtle red flags can be crucial in catching the problem early and potentially improving reproductive outcomes.
Surgical Diagnosis: Weighing the Benefits and Risks
While non-invasive imaging and blood tests continue to improve, definitive diagnosis of endometriosis often requires laparoscopy—an invasive surgical procedure that allows doctors to look inside the pelvic cavity. Although laparoscopy is a trusted method, it is understandably nerve-wracking for many patients given its invasive nature.
It is important to note that laparoscopy is not only a diagnostic tool but also a means of treatment. During the procedure, surgeons can remove or reduce the size of endometriotic lesions, which in some cases leads to an improvement in fertility. For many patients, having the option to both diagnose and treat the condition in one surgery is a super important advantage.
Improved Conception Outcomes in Endometriosis: Sorting Out the Little Twists of Fertility Data
A recent large-scale study involving over 4 million women over a span of 30 years in England illuminated a curious fact: while endometriosis increased the odds of infertility by two times, paradoxically, once diagnosed, patients with this condition were found to have up to a fourfold increased chance of conception compared to those with other causes of infertility.
Analyzing the Study Findings and Their Implications
The research, presented at the 41st Annual Meeting of the European Society of Human Reproduction and Embryology (ESHRE), provided a deep dive into the fertility outcomes among women with varying causes of infertility. Approximately 6.1% of the infertility cohort had surgically confirmed endometriosis, and a significant majority of these women had experienced infertility dilemmas before receiving a diagnosis.
Some of the key insights from the study include:
- A notable increase in conception rates among patients with endometriosis compared to those with tubal factors, ovulatory dysfunction, or unexplained infertility.
- The suggestion that early recognition and treatment could be contributing factors to these improved outcomes.
- Evidence indicating that surgical intervention, such as laparoscopic removal of endometriotic lesions, may enhance the odds of achieving pregnancy.
- A reminder that the condition’s presentation is varied, meaning that women with milder forms might maintain a high level of reproductive functionality when the disease is managed promptly.
These findings bring not only reassurance but also a renewed focus on patient education and early intervention as key components in managing endometriosis. For healthcare practitioners, the data encourages an approach that includes timely referrals for fertility counseling and early diagnostic procedures. Importantly, making your way through the challenging bits of endometriosis management involves both patient empowerment and individualized care strategies.
How Early Diagnosis Can Pave the Way for Better Fertility Outcomes
One of the most compelling aspects of the recent study is how early diagnosis plays a role in improving fertility outcomes. Women who become aware of their condition sooner are more likely to receive targeted treatments that can mitigate the negative impact of the disease on conception. This includes lifestyle modifications, medical therapies, and surgical options that tackle the problem before the condition causes lasting damage.
In cases where surgical intervention is appropriate, laparoscopic surgery can help by removing endometriotic lesions and reducing pelvic scarring. This intervention not only improves pain symptoms but can also reestablish a more favorable environment for conception. When combined with assisted reproductive techniques, these treatments could be key to boosting conversion rates for patients who might otherwise face significant fertility challenges.
Fertility Counseling and Tailored Treatment: Crafting a Personalized Plan
In light of the evidence linking endometriosis with better-than-expected fertility outcomes, a critical area that deserves attention is fertility counseling. For many women, discussing the implications of their diagnosis and weighing treatment options is a nerve-racking but necessary step in planning a future family.
One-on-One Consultations: What to Expect
The foundation of effective fertility counseling is clear, empathetic communication between the patient and the healthcare provider. During these consultations, patients are encouraged to express their concerns while receiving information on the likelihood of conception, particularly in comparison to other infertility challenges. Counselors provide insights not only about the condition itself but also about how interventions—both natural and surgical—can influence reproductive success.
Key components of a comprehensive fertility counseling session include:
- Reviewing the patient’s medical history and previous treatments.
- Discussing the findings of any diagnostic tests, including surgical confirmations of endometriosis.
- Outlining potential treatment plans and timelines, especially the benefits and limitations of laparoscopic surgery.
- Setting realistic expectations regarding conception and managing emotional and physical health before, during, and after treatment.
This personalized approach ensures that women with endometriosis can make informed decisions based on a clear understanding of their unique challenges and the available treatment options. It also helps demystify the condition, steering patients away from unnecessary anxiety by offering hope in the form of data-backed outcomes.
Addressing Age-Related Concerns in Fertility Outcomes
While endometriosis itself plays a significant role in the challenges of conception, other factors, notably age, remain critical to understanding fertility outcomes. Women in their 30s, particularly those aged 30 to 39, often face additional hurdles because fertility naturally declines with age. However, for those diagnosed with endometriosis, early intervention and the resulting improved conception rates provide a counterbalance to the intimidating effects of aging on fertility.
Healthcare providers emphasize an integrated approach that considers both the physiological and emotional aspects of the journey. When younger patients receive a diagnosis early, they can look at a broader range of treatment options, including both medical therapies and reproductive technologies, to help manage the condition while planning for parenthood.
Exploring Treatment Options: From Laparoscopy to Assisted Reproduction
There is no one-size-fits-all solution when it comes to managing endometriosis. Treatment plans must be tailored to the individual, taking into account the severity of the disease, the patient’s overall health, and their family planning goals. The following sections outline several treatment options available to women battling this condition and hoping for a successful pregnancy.
Surgical Management: Laparoscopy and Its Role in Improving Fertility
Laparoscopy has long been considered a cornerstone in diagnosing and treating endometriosis. Despite the nerve-wracking nature of a surgical procedure, many patients find solace in knowing that the surgery may not only alleviate painful symptoms but also enhance their overall fertility. During laparoscopy, a small camera is inserted through a minor incision, enabling surgeons to view the pelvic organs directly, diagnose endometriosis with precision, and remove problematic lesions.
Benefits of laparoscopic surgery include:
- Removal of endometriotic tissue, which can reduce inflammation and pain.
- Restoration of normal anatomy by freeing adhesions and scar tissue.
- Potential improvement in conception rates due to a healthier pelvic environment.
- Shorter recovery times and minimized surgical trauma compared to open surgery.
Even though surgery is not a guaranteed fix, when timed right and followed by supportive fertility treatments, it can be a super important step in optimizing reproductive outcomes. Many specialists also combine surgical and non-surgical approaches, using medications and lifestyle interventions to manage the condition holistically.
Assisted Reproductive Technologies: Beyond Natural Conception
For some patients, natural conception after an endometriosis diagnosis might require additional support. Assisted reproductive technologies (ART), such as in-vitro fertilization (IVF), can be an effective adjunct to natural conception, particularly when endometriosis is associated with other infertility factors. ART offers a way to bypass some of the tangled issues that may arise from anatomical distortions or the presence of adhesions.
When considering ART, patients and providers review a variety of factors, including:
- The patient’s age and ovarian reserve.
- The severity of the endometriosis and extent of pelvic damage.
- The potential benefits of combining surgical management with fertility treatments.
- The overall timeline for attempting conception and the urgency of treatment.
This comprehensive approach underscores how critical it is for patients to have multiple options at their disposal. Whether opting for natural conception bolstered by surgical intervention or leveraging the benefits of assisted reproduction directly, customized care paves the way for improved outcomes and a more hopeful future.
Patient Stories and Expert Perspectives: Digging into Real-Life Experiences
Personal narratives and expert insights are invaluable when making sense of the confusing bits related to endometriosis and its impact on fertility. Hearing the voices of those who have navigated this path can offer comfort, practical guidance, and a sense of community. Many women report that being proactive in seeking early treatment not only enhances their fertility prospects but also fuels a more positive outlook on life despite their diagnosis.
Real-World Experiences: Lessons Learned from Endometriosis Journeys
Patients who have successfully managed endometriosis and achieved pregnancy often emphasize the importance of recognizing early signs and seeking timely intervention. For some, the journey began with seemingly minor details such as progressive pelvic pain or irregular bleeding that eventually spurred them to consult a healthcare provider. These experiences underscore the need to not dismiss early symptoms as mere inconveniences.
Key takeaways from patient experiences include:
- Early consultation with a specialist can lead to a prompt and precise diagnosis.
- Surgical interventions, while intimidating at first, can offer both symptom relief and improved fertility outcomes.
- Fertility counseling is a crucial component of the journey, helping patients understand their options and set realistic goals.
- Emotional support, whether through counseling or patient support groups, is essential for managing the nerve-wracking aspects of the diagnosis and treatment process.
These stories remind us that despite the many little twists and uncertain spots that come with endometriosis, there is also a bright side. With the right support system and an early intervention strategy, women can turn a challenging diagnosis into an opportunity for proactive, personalized care that paves the way for successful conception.
Expert Insights: What Clinicians Want Patients to Know
Medical experts stress that while the road to conception for those with endometriosis may be full of problems, advancements in both diagnostic techniques and treatment methods have made it easier than ever to get around the more intimidating aspects of the condition. Clinicians advise that:
- Early detection is key—pay attention to your body’s signals, even if they seem like typical menstrual discomfort.
- Surgical interventions, especially laparoscopic surgery, have evolved tremendously, reducing both recovery times and potential complications.
- A multidisciplinary approach, incorporating surgical, medical, and assisted reproductive treatments, tends to yield the best outcomes.
- Fertility counseling should be an integral part of the treatment plan, helping to balance the physical and emotional demands of managing endometriosis.
Experts further emphasize that having a detailed conversation about treatment options can make the difference between feeling overwhelmed and feeling empowered. With personalized care plans tailored to each individual’s circumstances, the goal is to transform the overwhelming aspects of endometriosis into manageable pieces that lead to successful pregnancy outcomes.
Moving Forward: Balancing Treatment Strategies with Lifestyle Adjustments
As awareness about endometriosis and its potential effects on fertility grows, so does the emphasis on integrating medical treatments with changes in lifestyle. While clinical interventions such as surgery and ART are central to managing the condition, many patients find that complementary lifestyle adjustments can further improve their overall well-being and fertility prospects.
Lifestyle Modifications That Can Make a Difference
Women dealing with endometriosis often adopt a holistic approach that includes thoughtful dietary changes, regular exercise, and stress management techniques. Incorporating these measures into one’s routine might seem like a small step, but they can be key in mitigating the inflammatory aspects of the condition and fostering a healthier reproductive environment.
Some lifestyle strategies that have been reported to help include:
- A balanced diet: Emphasizing whole foods, lean proteins, fruits, and vegetables can help reduce inflammation.
- Regular physical activity: Moderate exercise, such as walking or yoga, can help manage weight and alleviate pelvic discomfort.
- Stress reduction: Techniques including meditation, deep breathing exercises, or even support groups provide avenues for reducing stress levels.
- Sleep hygiene: Consistent, high-quality sleep is essential for overall health and helps regulate hormonal balance.
While these lifestyle adjustments are not a cure, they do represent essential steps that can enhance overall treatment outcomes. By incorporating such strategies, patients create an environment where medical interventions may have an even better chance of success.
Integrative Therapies: Exploring Complementary Approaches
In addition to conventional medical treatments, several integrative therapies have shown promise in managing endometriosis symptoms. Acupuncture, for example, has been used by some patients to help alleviate pain and reduce stress. Herbal remedies and supplements, when used under proper medical guidance, may also offer relief from chronic inflammation and hormonal imbalances—both of which are common in women with endometriosis.
It is important to note that integrative therapies should be viewed as a supplement to, not a replacement for, traditional treatments. The aim is to create a well-rounded, personalized strategy that addresses both the physical and emotional challenges of endometriosis, thereby increasing the overall chance of conception.
Conclusion: Empowering Women Through Knowledge and Proactive Care
The journey through endometriosis is undoubtedly strewn with challenging parts and unexpected twists. Yet, the emerging evidence that women with endometriosis might have a higher chance of conceiving compared to those with other infertility causes offers a ray of hope. This counterintuitive finding underscores the importance of early detection, personalized fertility counseling, and comprehensive treatment planning.
Patients are encouraged to get into open dialogue with their healthcare providers about their symptoms, treatment options, and realistic expectations for conception. Whether it means opting for laparoscopic surgery, exploring assisted reproductive techniques, or making lifestyle adjustments, each step taken is a move toward regaining control over one’s reproductive future.
In an era of rapidly evolving medical research, the landscape of fertility and endometriosis is continuously being reshaped. With more awareness comes the promise of new treatment strategies—ones that not only address the nerve-wracking aspects of the diagnosis but also empower women to find their path toward parenthood. While the condition may be riddled with challenges and intimidating uncertainties, it also presents an opportunity to harness proactive care strategies that ultimately make conception a more achievable goal.
For clinicians and patients alike, these findings are a reminder that managing a complex condition is as much about understanding the condition’s natural progression as it is about employing modern medical tools to enhance the journey toward pregnancy. By working through the tangled issues with compassion, clarity, and evidence-based care, women encountering endometriosis can transform a daunting diagnosis into a gateway for informed reproductive decision-making.
Ultimately, education, timely intervention, and holistic treatment are the cornerstones of managing endometriosis and its effects on fertility. The unexpected silver lining—that women with this condition might experience higher conception rates than those suffering from other infertility issues—serves as a testament to the power of early intervention and personalized care. It encourages both patients and providers to steer through the complicated pieces together, ensuring that every woman feels supported and informed as she embarks on this unique journey.
In conclusion, it is essential to continue researching and sharing knowledge about the subtle details and small distinctions in how endometriosis affects fertility. With ongoing studies and increased patient awareness, the fine points of this condition continue to be unraveled, and more positive outcomes are on the horizon. For those facing the nerve-wracking challenges of endometriosis, there is now a scientific foundation to support informed, proactive care that transforms a traditionally off-putting diagnosis into a hopeful pathway towards parenthood.
As we move forward, let us keep in mind that every twist and turn in the journey of endometriosis is an opportunity to learn, adapt, and ultimately thrive. With the right mix of medical expertise, compassionate counseling, and integrative lifestyle strategies, women can navigate the fine details of their fertility challenges and look forward to a future filled with promising possibilities.
At its core, this evolving story is about more than just fertility rates—it’s about empowering women to take charge of their reproductive health, confidently make their way through the overwhelming bits, and embrace their potential for a fulfilling family life. The road may be long and full of confusing bits, but with perseverance, support, and a dedication to comprehensive care, the journey becomes one of resilience and hope.
The conversation surrounding endometriosis and fertility is continually evolving, and every new study brings us a step closer to unraveling the hidden complexities of this condition. It’s a reminder to all women that even when faced with challenging diagnoses, there is light at the end of the tunnel—a light fueled by scientific discovery, patient advocacy, and a relentless commitment to turning daunting challenges into achievable dreams.
Originally Post From https://www.contemporaryobgyn.net/view/endometriosis-linked-to-higher-pregnancy-rates-vs-other-infertility-causes
Read more about this topic at
Unexplained Infertility: Tests, Diagnosis & Treatment
Spontaneous Pregnancy and Unexplained Infertility
