Recent Developments in HIPAA and Reproductive Health Information Privacy
The recent U.S. District Court decision in the Purl case has stirred up a storm in the realm of health care privacy. This opinion editorial examines the ruling that vacated key provisions of the HIPAA Final Rule related to reproductive health information privacy, and what this means for HIPAA-covered entities. In our discussion, we will take a closer look at the background of the Final Rule, review the decision’s legal rationale, and explore how regulated entities can adjust their compliance programs to steer through the new landscape.
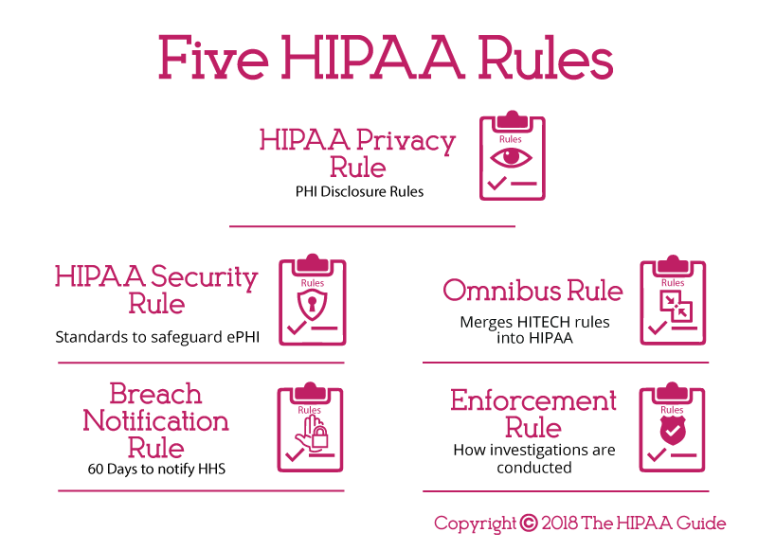
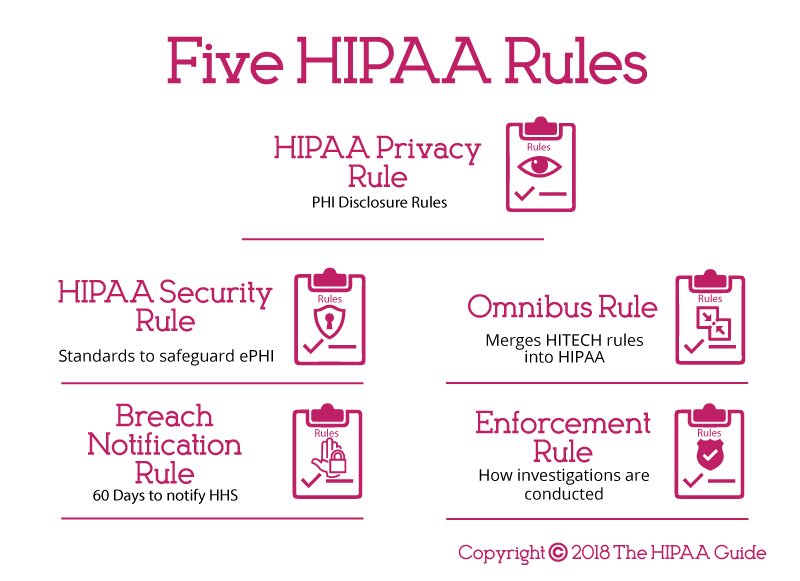
Background of HIPAA and the Controversial Final Rule
In response to significant legal shifts after the Dobbs v. Jackson Women’s Health decision – which overturned Roe v. Wade – the U.S. Department of Health and Human Services (HHS) sought to shore up privacy protections for sensitive reproductive health care information. On April 22, 2024, HHS OCR issued what is known as the Final Rule, a set of modifications to the HIPAA Privacy Rule. Designed to limit the use and disclosure of protected health information (PHI) tied to reproductive care, the rule introduced several new requirements for health care providers, health plans, and health care clearinghouses.
This new rule was intended to enhance the privacy of reproductive health data by disciplining the circumstances under which such sensitive PHI could be shared for non-health care purposes. It also imposed the requirement for obtaining a signed and dated attestation from parties requesting reproductive health-related PHI in healthcare oversight, judicial, administrative, and enforcement scenarios. Additionally, regulated entities were mandated to update their Notice of Privacy Practice (NPP) to reflect these changes. However, critics argued that the attestation process involved tricky parts and tangled issues that could overwhelm providers with extra administrative burdens.
Table 1 outlines the main components of the Final Rule introduced by HHS OCR in 2024:
| Component | Description |
|---|---|
| PHI Usage Restrictions | Limited circumstances for non-health care disclosures related to reproductive health. |
| Attestation Requirement | Mandatory signed and dated attestation for accessing reproductive health-related PHI. |
| NPP Updates | Revised Notice of Privacy Practice to increase privacy protections for reproductive health care information. |
Despite the intended benefits of safeguarding reproductive health data, many stakeholders found that the rule presented a series of complicated pieces and confusing bits, especially regarding the attestation requirement.
Court Ruling and Its Legal Implications
On June 18, 2025, the U.S. District Court for the Northern District of Texas (Amarillo Division) rendered a decision in the case of Purl v. Department of Health and Human Services. The court ruled that the portions of the Final Rule meant to enhance reproductive health privacy – except for changes related to 42 C.F.R. Part 2 concerning substance use disorder records – were unlawful. This decision effectively vacated most of the Final Rule on a nationwide basis.
The court’s verdict was based on several key points, each revealing subtle details about regulatory overreach and statutory authority. Here are the main reasons behind the decision:
- Interference with State Laws on Child Abuse Reporting: The court found that the rule’s blanket prohibition on sharing PHI for reproductive health care, along with its burdensome attestation requirements, unlawfully restricted state child abuse reporting laws. This interference with state mandates was seen as a serious misstep.
- Exceeding Statutory Authority: The court argued that HHS ventured too far by redefining statutory terms such as “person” and “public health,” thus exceeding its legally granted authority.
- Lack of Congressional Backing: The court noted that there was no clear congressional mandate authorizing HHS to regulate highly sensitive and politically charged subjects like abortion and gender-affirming care.
These points not only expose the tangled issues inherent in the Final Rule but also highlight the challenges of imposing additional layers of bureaucracy on sensitive health information. The ruling signals that while ensuring privacy is essential, the methods used by federal agencies must align clearly with both statutory authority and the established frameworks of state laws.
Implications for HIPAA-Covered Entities: Challenges and Opportunities
For health care providers, health plans, and health care clearinghouses – collectively known as regulated entities – the Purl decision necessitates a careful reassessment of compliance programs. The immediate effect is that many of the previously mandated complex procedures, like obtaining attestations for PHI requests related to reproductive care, are no longer required. This change frees entities from certain intimidating procedures and offers an opportunity to revise internal policies in a more streamlined way.
Below are some key recommended steps for regulated entities as they update their HIPAA compliance programs:
- Revise Internal Policies and Procedures: Ensure that all documents, including training materials and response protocols for PHI requests, are aligned with the current HIPAA Privacy Rule as modified by the Purl ruling. Removing outdated references to the attestation requirement is crucial.
- Update Business Associate Agreements (BAAs): Review and, if necessary, amend BAA forms to eliminate any clauses that mention the attestation process.
- Reassess Notice of Privacy Practice (NPP): While the revisions related to substance use disorder records remain in effect, decide if further updates are needed based on evolving legal interpretations.
- Continuous Monitoring and Training: Conduct regular reviews of HIPAA compliance practices and provide updated training for staff to ensure they understand the current legal framework.
Each of these steps represents a tactical move to simplify compliance procedures—a welcome change for many in the health care industry dealing with the daunting administrative maze that previously existed.
Understanding the Attestation Requirement: Tangled Issues and Alternatives
One of the most contentious aspects of the disputed Final Rule was the mandatory attestation requirement. Under the rule, regulated entities were obliged to secure a signed and dated statement from any individual or entity seeking access to reproductive health-related PHI for purposes ranging from health care oversight to law enforcement. This particular stipulation was viewed by many as a nerve-racking and intimidating addition, laden with loopholes and excessive paperwork.
Critics of the requirement argued the following:
- The process was overly burdensome, creating significant delays in accessing important information for necessary oversight activities.
- The attestation form was not user-friendly and often involved convoluted legal language, making it hard to understand and implement.
- Entities faced a high risk of non-compliance due to the sheer volume of requests and the conflicting interpretations of what constituted “reproductive health care information.”
As a result of the Purl decision, the attestation requirement has been scrapped for all practical purposes (with the exception of provisions under 42 C.F.R. Part 2). This removal represents a move towards a more balanced approach where respondents no longer need to navigate the twists and turns of this particularly confusing piece of regulation.
Compliance Updates: Key Considerations for Health Care Providers and Partners
In the wake of the court’s decision, HIPAA-covered entities are tasked with re-evaluating and adjusting their compliance frameworks. This is not merely a matter of updating paperwork, but of rethinking how sensitive health information is managed, especially as it relates to reproductive care. Regulatory professionals now have the opportunity to craft policies that are both legally sound and operationally efficient.
Below are some key points that providers should keep in mind during this transition:
- Streamlining Procedures: Remove convoluted steps that were introduced under the Final Rule, ensuring that requests for reproductive health-related PHI are processed in line with the current HIPAA requirements.
- Staff Re-Training: It is essential to educate employees about the changes. Training sessions should focus on revising the misunderstood or overly complex parts of the previous rule.
- Document Revisions: Update internal manuals, compliance checklists, and training guides to reflect the new procedures. Ensure that references to the outdated attestation process are eliminated.
- Communication With Business Partners: Inform business associates and partners of the change to avoid any confusion over compliance obligations. This step helps maintain a consistent approach across all related operations.
Furthermore, clear documentation that outlines these revisions will help mitigate any potential legal misunderstandings in the future. For example, using checklists and flowcharts to clearly define the new process for PHI requests can significantly reduce the chances of misinterpretation. Such tools act as a roadmap that helps regulated entities find their way through the updated compliance landscape.
Differences Between Federal and State Regulations: Finding Your Path Through Jurisdictional Challenges
The Purl decision has reignited the debate over federal versus state jurisdiction in regulating sensitive health matters, particularly in areas as hotly contested as reproductive health care. On one hand, HHS’s attempt to set nationwide standards through the Final Rule was seen by many as a necessary measure to boost privacy protections. On the other, state officials – supported by multiple legal challenges – contend that such a one-size-fits-all approach intrudes on their authority to enforce state-specific laws on child abuse reporting and other protective measures.
This discrepancy creates a situation where:
- State authorities believe in their right to manage local reporting procedures: Many states argue that they should retain control over how child abuse investigations and other sensitive issues are handled within their jurisdictions.
- Federal efforts aim to standardize practices: HHS’s approach intended to ensure that regardless of state lines, all individuals receive consistent privacy protections for their reproductive health information.
For regulated entities that operate across multiple states, the challenge is to reconcile these differing expectations. Providers must now carefully review both state and federal guidelines, ensuring that they are fully compliant with local requirements while taking advantage of the streamlined federal rules post-Purl. This balancing act means staying alert to ongoing legal challenges and adjustments that may require further modifications to internal policies.
Challenges and Opportunities in Revising HIPAA Policies
The immediate task for HIPAA-regulated entities is to update existing policies to reflect the current legal environment. This means revising procedural documents, operational manuals, and even digital workflows to ensure that they no longer refer to the vacated attestation requirement. However, amidst these procedural modifications lie opportunities for improvement.
Entities should consider these factors when revising their policies:
- Clarity and Precision: Use plain language and avoid legal jargon. Providers should replace complicated language with simpler expressions to outline essential steps.
- Consistency Across Documents: All references in training manuals, BAAs, and internal policies must be harmonized to reflect the current HIPAA Privacy Rule. This prevents confusion and ensures that all team members are on the same page.
- Operational Efficiency: With the removal of certain burdensome requirements, there is a chance to develop quicker response mechanisms for processing PHI requests. This can lead to reduced administrative overhead and a more agile compliance framework.
- Risk Mitigation: Clear policies help reduce the risk of non-compliance. In a landscape where legal interpretations can change rapidly, a well-documented framework serves as a shield against potential legal challenges.
In practical terms, regulated entities can benefit from creating visual aids such as process maps or flow diagrams. For instance, a simple flowchart illustrating the steps that need to be taken when receiving a PHI request can demystify the process and ensure that staff do not get lost in the twists and turns of compliance updates.
Below is an example outline for revising internal HIPAA policies:
- Analyze existing guidelines to identify outdated references.
- Collaborate with legal counsel to ensure updates are in line with the current HIPAA Privacy Rule.
- Engage staff with training sessions that incorporate practical examples and decision trees.
- Implement regular audits to ensure compliance with the new standards.
By taking these steps, health care providers can transform what may initially seem like an overwhelming overhaul into a series of manageable, step-by-step improvements.
Broader Perspectives on Reproductive Health Data Privacy
This unfolding legal drama is not just about compliance—it raises important questions regarding the balance between individual privacy and the need for oversight in sensitive areas like reproductive health care. The decision to invalidate major parts of the Final Rule underscores the tension between federal attempts to enforce uniform privacy standards and the nuanced, often state-specific realities on the ground.
On one side of the debate, advocates for enhanced privacy measures argue that any relaxation in guidelines threatens personal autonomy and the confidentiality of reproductive health data. On the other, critics contend that overly aggressive federal mandates can obstruct other critical areas, such as child abuse reporting and state-level protections. This situation is full of problems when trying to achieve a balance, as both federal and state bodies strive to uphold their respective mandates.
In our view, there is a need for a measured approach that does not impose overly intimidating administrative burdens on health care providers while still protecting patient privacy. More importantly, any regulatory framework should be adaptable to the shifting legal and social landscapes. This means that future iterations of HIPAA-related policies must account for both the fine points of federal regulations and the small distinctions that exist across various states.
Comparative Insights: Federal vs. State Approaches to Health Data Privacy
The divergence between federal initiatives and state regulations is a recurring theme in the ongoing debate over reproductive health care privacy. The vacated provisions of the Final Rule have left many state-level regulatory actions intact. However, several lawsuits are still pending, with states like Texas, Tennessee, and Missouri pressing back against perceived federal overreach.
When trying to figure a path forward, it is important to consider the following points:
- State Authority and Sovereignty: Many states contend that they possess the necessary independence to enforce child abuse reporting laws and other related regulations. They argue that a blanket federal requirement undermines state autonomy.
- Impact on Enforcement: The state-led lawsuits specifically focus on how the Final Rule might obstruct local investigative efforts. This spotlight on enforcement reveals the nerve-racking challenges that arise when trying to harmonize local and national legal standards.
- Long-Term Regulatory Trust: For regulated entities, consistency in the rules they must follow is key. The ongoing legal disputes contribute to an environment of uncertainty, making it crucial for entities to remain flexible and vigilant.
To help illustrate these contrasts, the following table offers a snapshot of the differences between the federal and state perspectives on reproductive health information privacy:
| Aspect | Federal Approach (Final Rule) | State Standpoint |
|---|---|---|
| Privacy Protection | Enhanced protection through mandatory attestations and revised NPPs. | Variable; states prefer controls that do not impede child abuse reporting. |
| Administrative Burden | High due to additional documentation requirements. | Prefer streamlined procedures that align with state-specific reporting laws. |
| Jurisdictional Authority | Uniform federal mandates aimed at nationwide consistency. | Emphasizes state autonomy and localized enforcement mechanisms. |
This snapshot highlights the significant differences and underlines the need for a policy approach that respects both federal intentions and state prerogatives.
Future Outlook on HIPAA Reforms and Reproductive Health Information Security
The reversal of key provisions of the Final Rule by the Purl decision raises questions about future directions for HIPAA reform in the realm of reproductive health privacy. Although the attestation requirement is off the table, the underlying issues concerning the balance between patient privacy and public safety remain unresolved. Stakeholders on both sides of the debate are poised for further legal, administrative, and legislative actions.
Consider these potential directions for future reform:
- Legislative Clarification: Congress may need to step in to provide clearer guidelines addressing the proper balance between patient privacy and state enforcement needs. Future laws could reduce the room for interpretation that led to the current legal challenges.
- Technological Advancements: As technology evolves, there may be new ways to protect sensitive health data without burdening regulated entities with nerve-racking paperwork. Digital authentication methods and secure data-sharing platforms could emerge as alternatives.
- Interagency Cooperation: A collaborative effort between federal agencies and state governments can help align the different priorities. This could lead to policies that are both flexible and effective, allowing for localized enforcement without undermining fundamental privacy protections.
- Ongoing Legal Review: As more cases reach the courts, both the Federal and State judicial systems will continue to offer interpretations on how best to safeguard reproductive health information. Regulated entities must be prepared for further updates and clarifications.
The overall outlook is one of cautious optimism. While the recent decision eliminates some of the more intimidating administrative requirements set forth by the Final Rule, it also opens the door to ongoing debates regarding privacy, state authority, and compliance. For regulated entities, the challenge will be to continuously monitor these changes and update internal policies accordingly to stay on the right side of the law.
Reflections on the Role of Regulatory Agencies in Health Care Privacy
At its core, the debate over the HIPAA revisions and the Purl decision emphasizes the delicate balance that regulatory agencies have to strike. On one side is the imperative to protect sensitive health information—a matter that is super important for patient trust and privacy. On the other side lies the need to ensure that such protections do not inadvertently hamper critical state functions, such as the reporting and investigation of child abuse cases.
This balancing act is undoubtedly full of problems, especially when the stakes involve both personal privacy and public safety. There are several considerations that regulatory bodies must keep in mind:
- Transparency: Agencies need to adopt transparent rule-making processes that clearly communicate the rationale behind introducing or retracting certain regulations. This openness is key to building trust among stakeholders.
- Stakeholder Engagement: Engaging with both health care providers and state officials during the rule-making process can help merge fine shades of policy with practical realities. Regular feedback can steer policy in directions that are both legally sound and operationally feasible.
- Flexibility: Policies must leave room for adjustments as societal values, technology, and legal interpretations evolve. This flexibility is especially critical in areas with such nerve-racking social and political implications.
In reflecting on these issues, it becomes clear that the role of regulatory agencies—even those with a broad federal mandate—is not to impose rigid restrictions, but rather to facilitate a framework that adapts to the changing environment of health care privacy.
Key Recommendations for Regulated Entities Moving Forward
For the multitude of health care providers, health plans, and clearinghouses impacted by these changes, the following recommendations can offer guidance as they work through revising compliance protocols:
- Conduct a Comprehensive Compliance Audit: Begin by reviewing all internal policies, training materials, and BAAs to identify any references to the vacated attestation requirements. A clear audit helps isolate the nerve-racking elements that need removal.
- Update Training and Documentation: Organize re-training sessions for staff to familiarize them with the new compliance landscape. Using clear examples and flow charts can make it easier for employees to grasp the necessary adjustments.
- Establish a Monitoring System: Regular internal reviews and audits, perhaps facilitated by digital monitoring tools, can help catch any discrepancies or lapses in adherence to the updated HIPAA Privacy Rule.
- Engage in Legal Consultation: Given the ongoing legal debates, it is wise to consult with legal experts who specialize in health care privacy. This will ensure that any new guidelines are not only clear of the twists and turns of deprecated rules but are also fully compliant with both federal and state laws.
- Prepare for Further Changes: Stay informed about new court decisions and legislative actions that might affect HIPAA compliance. Proactively updating policies can help mitigate the risk of future legal complications.
Adopting these recommendations not only helps in mitigating risk but also positions entities to respond swiftly to any subsequent legal or regulatory shifts. In many ways, this is an opportunity to move away from rigid frameworks toward a more dynamic and responsive organizational policy culture.
Conclusion: A Call for Balanced and Adaptive Compliance
The Purl decision represents a turning point in the ongoing debate over reproductive health information privacy. By vacating significant parts of the HIPAA Final Rule, the court has signaled that while robust privacy protections for sensitive health data are essential, they must not come at the expense of interfering with state authority or imposing overly intimidating administrative burdens on health care providers.
For regulated entities, this means a reprieve from complex and nerve-racking attestation processes and a chance to simplify internal compliance measures. However, it also calls for a careful re-examination of how best to align internal policies with both the current HIPAA Privacy Rule and broader legal expectations. With differences between state and federal guidance still evident, providers must keep their policies flexible, transparent, and informed by ongoing legal interpretations.
Looking forward, the future of HIPAA reforms rests on achieving a balance that safeguards patient privacy while ensuring that necessary state functions, like child abuse reporting, remain uncompromised. As legal challenges continue to surface and further adjustments are made at the legislative level, health care providers would do well to continuously review and update their compliance frameworks, ensuring that they are both compliant and efficient.
In summary, the vacating of the contentious provisions within the Final Rule invites a more streamlined and adaptive compliance environment. It is a crucial reminder that as our legal and social landscapes evolve, so too must the frameworks that govern key aspects of personal health information. By embracing these necessary changes and preparing for future adjustments, HIPAA-regulated entities can confidently move forward while preserving the essential balance between privacy and accountability.
Originally Post From https://www.jdsupra.com/legalnews/u-s-district-court-ruling-vacates-hipaa-3563052/
Read more about this topic at
Federal Court Strikes Down HIPAA Reproductive Health …
HIPAA’s Reproductive Health Rule Is Vacated Nationally