An Opinion on Evolving Treatment Strategies for Low Sexual Desire in Women
This editorial explores the latest guidelines for treating low sexual desire in women—a medical condition that is both common and often misunderstood. At the center of these developments is a consensus paper led by experts at the University of California San Francisco (UCSF). The new recommendations cover a range of treatment options, including medication-based therapies, hormone treatments, and various psychological interventions. In this opinion piece, we take a closer look at these guidelines, discuss the benefits and challenges of a biopsychosocial approach, and consider what it all means for women’s sexual health today.
A Closer Look at Low Sexual Desire and Its Impact
Low sexual desire, clinically known as Hypoactive Sexual Desire Disorder (HSDD), affects many women but is rarely addressed with the urgency it deserves. It can manifest as a reduced level of interest in sexual activity, a diminished response to erotic cues, or active avoidance of situations that might lead to intimacy. Such symptoms bring not only personal distress but also impact overall relationship satisfaction. The condition is surrounded by confusing bits of stigma and misinterpretation, underscoring the need for clear, evidence-based guidelines.
Evidence-Based Recommendations: A New Era in Women’s Sexual Health
For the first time, sexual medicine experts have come together to produce treatment guidelines that blend medical, psychological, and lifestyle approaches into a coherent strategy for managing HSDD. The UCSF-led international committee stressed that treatment options should be tailored to a patient’s specific goals while balancing risks and benefits. In their comprehensive consensus paper, published in Sexual Medicine Reviews, experts outlined a multifaceted treatment plan. By addressing both the physical and psychological aspects of low sexual desire, the guidelines aim to help providers find your way through a condition that has long been overlooked.
Broadening the Treatment Spectrum: Combining Medication and Hormone-Based Therapies
One of the key elements in the new guidelines is the use of medication-based treatments and hormone therapies to treat HSDD. These options are designed to act on the biological underpinnings of sexual desire, targeting hormonal imbalances and neurotransmitter activity that may be contributing to low libido. Although these strategies have shown promise, they come with tricky parts. For example:
- Risk/Benefit Analysis: Every treatment comes with potential side effects. Providers must weigh these against the benefits to ensure patient safety and satisfaction.
- Role of Hormones: Hormone therapies can be particularly effective for some women, but the response varies widely, making it important to personalize treatment plans.
- Medication Interactions: When combining treatments, it is essential to consider how different medications might interact—a process that can often feel intimidating.
This part of the treatment plan emphasizes the need for clear communication between providers and patients. Women should be informed about what each medication does, how it might affect their overall health, and what side effects they should expect. With this detailed approach, providers can help patients figure a path through the maze of treatment options with confidence.
Integrating Psychological Interventions in Sexual Health Management
The guidelines also highlight a range of psychological interventions as essential components to effectively treat HSDD. These non-medication strategies include sex therapy, cognitive behavioral therapy (CBT), and mindfulness-based therapy. Each of these approaches is geared toward addressing the subtle parts—the hidden complexities—of psychological and emotional distress that may accompany low sexual desire.
Sex Therapy: This therapy helps women explore and break down the emotional blocks that might be contributing to a lack of desire. It’s a chance to address personal insecurities and relationship issues in a safe and supportive environment.
Cognitive Behavioral Therapy (CBT): CBT focuses on changing negative thought patterns and behaviors that can interfere with a satisfying sexual life. It’s especially useful for those who find that negative self-perceptions or anxiety hinder their sexual expression.
Mindfulness-Based Therapy: By encouraging patients to remain present and engaged in the moment, mindfulness-based practices help counteract the scattered thoughts and worries that often interfere with sexual pleasure.
Understanding the Biopsychosocial Approach in HSDD Treatment
A central theme in the UCSF guidelines is the use of a biopsychosocial approach. This method considers not only the physical but also the social and emotional aspects of sexual health. In many ways, it offers a road map for addressing a condition that is loaded with issues on multiple levels. Here’s how the approach breaks down:
| Dimension | Description | Examples |
|---|---|---|
| Biological | Focuses on the physical and hormonal mechanisms | Medication, hormone therapy, neurotransmitter activity |
| Psychological | Addresses mental and emotional wellbeing | Sex therapy, CBT, mindfulness-based interventions |
| Social | Considers the relational and societal context | Relationship counseling, communication strategies |
This table provides an overview of how the multifaceted nature of HSDD is tackled. By acknowledging that sexual desire is influenced by a myriad of factors, providers can work through the tangled issues with greater precision and empathy.
Managing the Risk and Reward Balance: Patient-Centered Treatment Planning
One of the super important takeaways from the guidelines is the focus on patient-centered care. This means that every treatment recommendation must be carefully aligned with each patient’s personal goals and circumstances. The process involves a detailed risk/benefit discussion where the following factors are considered:
- Personal Goals: What does the patient hope to achieve—be it an increase in desire, a more fulfilling intimate life, or better emotional connection?
- Risk Assessment: Evaluating potential side effects or complications from medication and hormonal treatments.
- Psychological Readiness: Determining whether the patient is open to therapeutic interventions, which might sometimes feel overwhelming.
- Financial and Lifestyle Considerations: The feasibility of maintaining a certain treatment plan while balancing work, life, and other responsibilities.
This transparent dialogue helps ensure that treatment plans are not only medically sound but also practical and sustainable. In many ways, it represents a shift from a one-size-fits-all approach to a personalized road map where each patient’s unique situation is taken into account.
Challenges in the Implementation of New Guidelines
Introducing comprehensive guidelines for HSDD is undoubtedly a progressive step, but the path to widespread adoption is full of problems. There are several tricky parts that both providers and patients must work through:
- The Learning Curve: Many clinicians may find themselves needing additional training to fully understand and implement the nuanced recommendations. The fine points of these guidelines can seem overwhelming at first.
- The Stigma Surrounding HSDD: Sexual health issues often carry extra baggage from social taboo. This stigma can make it harder for patients to discuss their symptoms openly.
- Insurance and Cost Issues: Not all treatments, especially the psychological interventions, may be covered by insurance. This places a heavier load on patients who might already be feeling hesitant.
- Integration into Standard Practice: Healthcare systems may need to adjust their protocols and referral processes to accommodate this multi-faceted approach.
Despite these challenges, the guidelines represent a critical step toward addressing what has long been a neglected area of women’s health. The systematic review of available treatments and the individual-centered philosophy can help providers figure a path through the maze of possible interventions.
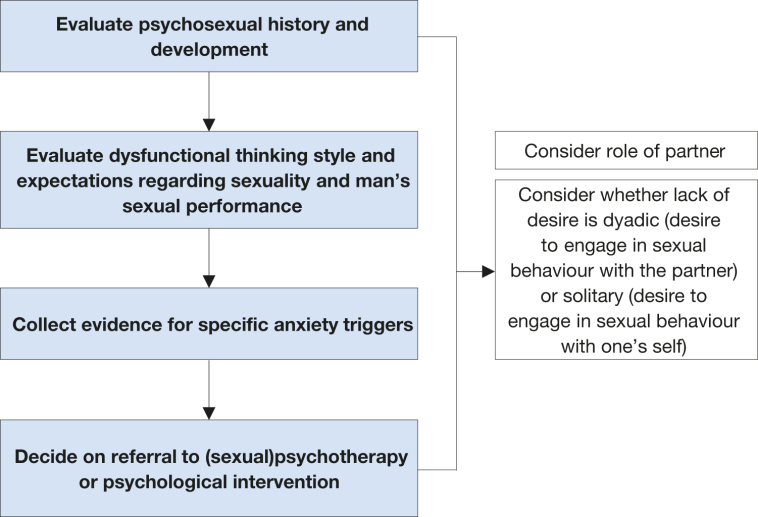
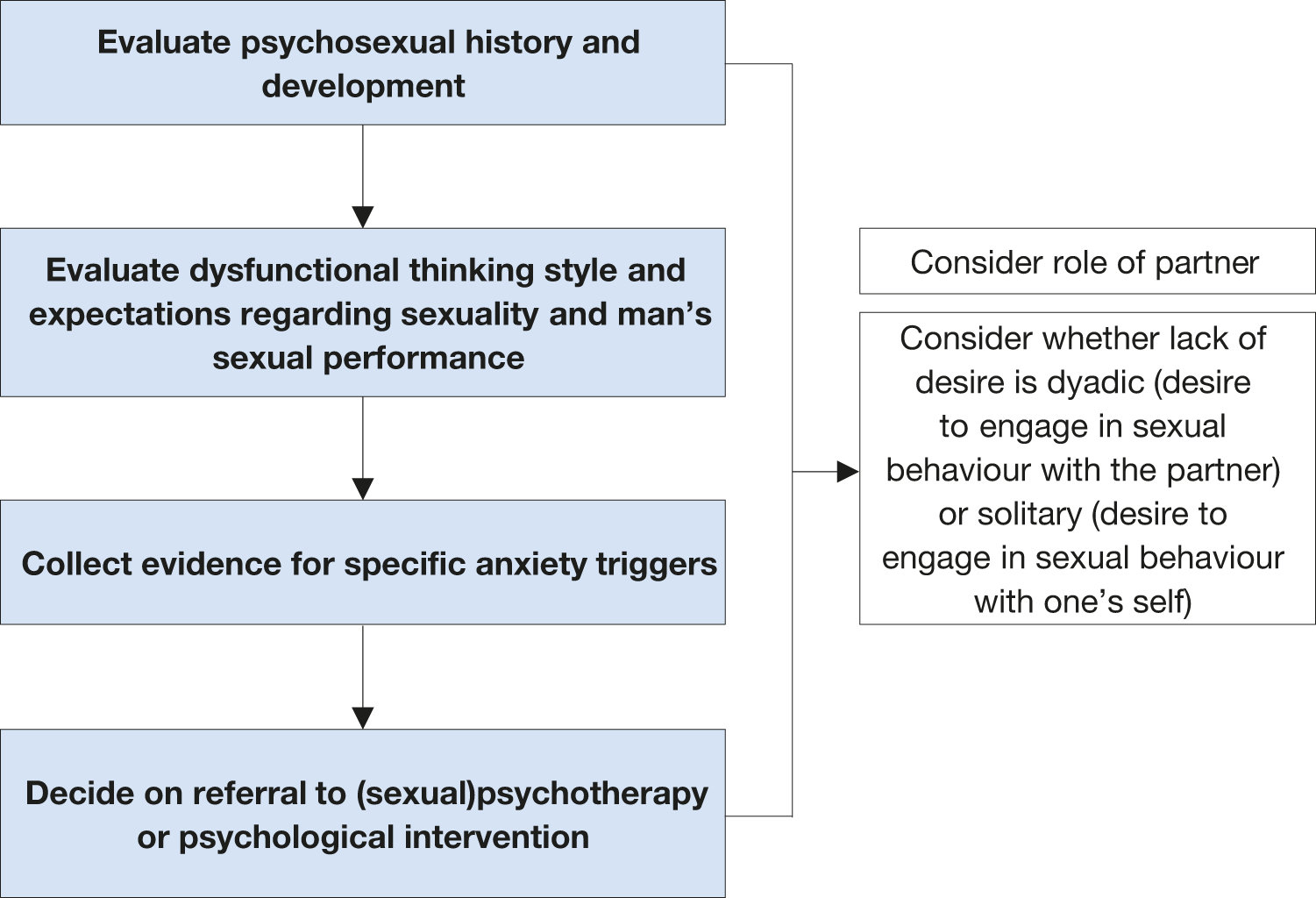
Psychological Interventions: Addressing the Emotional Landscape of HSDD
Let’s dig into the strategies that focus on the psychological side of the issue. Psychological interventions are not just add-ons to medication regimens; they act as the cornerstone of a balanced treatment strategy. For many women, mental and emotional factors are inextricably linked to physical symptoms. Here’s why these interventions are considered essential:
- Breaking Down Barriers: Psychological therapies help unearth and address long-standing negative views about sex. Many women might feel intimidated when considering their own desires due to cultural or personal beliefs.
- Empowering Patients: With therapies such as CBT, patients learn to challenge self-defeating thoughts and build confidence. This empowerment is a critical step toward reclaiming a sense of control over their sexual health.
- Enhancing Relationship Dynamics: Often, a strained connection with a partner can exacerbate or even trigger HSDD. Relationship counseling and sex therapy provide tools to improve communication and support both partners in their intimacy journey.
- Long-Term Benefits: Unlike some quick fixes, psychological approaches offer skills and insights that can lead to sustained improvement, ensuring that the benefits extend well beyond the treatment period.
Collectively, these psychological strategies help patients work through the tangled issues that might have developed over years. Instead of simply masking symptoms, they invite women to engage in a deeper, reflective process of healing and self-discovery.
Medication and Hormone Therapies: Understanding the Physical Interventions
Medications and hormone therapies address the biological components of low sexual desire. When used appropriately and tailored to an individual’s needs, these treatments can be transformative. However, it’s important to remember that these strategies are most effective when part of a broader, integrated plan. Here are some key considerations:
- Beneficial Outcomes: When correctly administered, medications can stimulate sexual desire and energy. Hormone therapies, on the other hand, work by rebalancing the body’s internal systems.
- Side Effects: Every treatment option comes with potential complications. Providers need to stay alert to the possibility of side effects, ensuring that any negative reactions are quickly managed.
- Customizing Treatment: Not all patients respond the same way. The key is to refine the approach—using detailed assessments and ongoing tracking—to understand what works best for each woman.
- Combining Treatments: Sometimes, the best results come from combining biomedical interventions with psychological approaches. For instance, a patient might benefit from both a low-dose hormone therapy and a regimen of mindfulness-based therapy to achieve a balanced outcome.
This section stresses that while medication and hormone therapy can be powerful tools, they are only one part of a comprehensive treatment plan. The challenge for clinicians lies in balancing these biomedical interventions with supportive therapies that address the emotional and social factors behind HSDD.
Patient Stories: The Human Side of HSDD Treatment
Although our focus is on the guidelines and the science supporting them, it’s important to recognize the human impact behind these recommendations. Many women who have experienced low sexual desire mention feeling isolated or misunderstood. A patient might describe her journey as being full of twists and turns, with each treatment option revealing new challenges and opportunities.
Consider the story of a woman who, after years of silence and self-doubt, finally sought help. With the aid of a tailored treatment plan that combined hormone therapy with cognitive behavioral therapy, she was able to rebuild her sense of intimacy and confidence. Her journey was filled with moments that were both scary and encouraging—each step requiring her to work through subtle differences and fine shades of her own experience. Stories like these underscore why it is so critical to have a well-rounded, patient-centered approach in place.
Implementing the Guidelines in Everyday Practice
Changing the way we treat HSDD is not just about drafting guidelines—it’s about putting these recommendations into practice. For many healthcare providers, figuring a path through this new approach might seem intimidating, but the benefits could be far-reaching. Practical steps for implementation include:
- Provider Training: Educational initiatives and continuing education courses are essential to help clinicians understand the full scope of these recommendations.
- Clinical Protocols: Developing standardized protocols can help ensure that every patient receives a comprehensive evaluation that considers both biological and psychological factors.
- Multidisciplinary Care: Collaboration between gynecologists, psychiatrists, sex therapists, and primary care professionals is needed to build a seamless care team for each patient.
- Patient Education: Informative resources, support groups, and counseling can empower women to understand their options and feel more confident in managing their treatment plans.
Tailoring these steps to fit the unique setting of each healthcare practice will not be without its tangled issues. However, the potential rewards—in terms of improved patient outcomes and greater provider satisfaction—make it a path worth taking.
The Future of Women’s Sexual Health: Benefits and Opportunities
The release of these guidelines represents a promising milestone in the ongoing evolution of women’s sexual health care. While the process of integrating new treatment strategies into daily practice is dotted with challenging bits and nerve-racking decisions, it also offers a rich opportunity for growth and improvement. As more providers begin to take a holistic, biopsychosocial approach, we can hope for a future where women feel more empowered, supported, and confident in discussing their sexual health.
One of the most significant benefits of these new guidelines is the recognition that there is no single solution for HSDD. Instead, success depends on a balanced combination of medical insight, psychological strategies, and ongoing communication between providers and patients. This integrated model encourages providers to work through the shared challenges and celebrate small distinctions that make a success story truly unique.
Key Takeaways for Providers and Patients Alike
In summary, the new treatment guidelines for Hypoactive Sexual Desire Disorder offer several critical lessons for both healthcare providers and patients:
- Comprehensive Care: An integrated treatment plan that includes biological, psychological, and social interventions is key to properly addressing HSDD.
- Personalized Approach: Treatments need to be tailored to the individual, taking into account personal goals, lifestyle, and the fine points of each case.
- Patient Education: Informing patients about what to expect from various treatment options helps them maintain a realistic outlook and active participation in their care.
- Interdisciplinary Collaboration: Bringing together experts from multiple fields is essential for managing the tangled issues and hidden complexities of the disorder.
- Ongoing Support: Demystifying the treatment process through transparency and continuous discussion can alleviate some of the intimidating aspects of managing HSDD.
These takeaways not only underline the importance of the new guidelines but also highlight the evolving nature of women’s sexual health care—a field that continues to grow with each new research finding and clinical insight.
Looking Back and Moving Forward: Reflections on the Guidelines
In reflecting on these guidelines, one can appreciate how far the field of sexual medicine has come. For years, HSDD was handled with a one-dimensional approach that often left patients feeling dismissed or misunderstood. Today’s recommendations recognize that improving sexual desire is a multi-layered process, requiring care that is as flexible as it is comprehensive.
It is important to remember that while these recommendations provide a robust framework, real-world application will likely reveal additional challenges. Factors such as cultural expectations, societal stigma, and individual variability mean that every case presents its own set of tangled issues. Health professionals must, therefore, be prepared to make adjustments and embrace a learning mindset, constantly asking themselves how best to support their patients through each nerve-racking twist and turn.
Addressing the Wider Social and Cultural Context
Beyond the clinical realm, these guidelines also invite us to address the wider social and cultural context of women’s sexual health. HSDD is not just a medical condition; it is deeply interwoven with issues of self-esteem, relationship dynamics, and social norms. By opening up informed conversations about sexual desire and wellbeing, the medical community is taking a crucial step toward de-stigmatizing a condition that has long been shrouded in silence.
The discussion helps bring subtle details to the forefront:
- Visibility: Recognizing that sexual health is an important aspect of overall wellness can encourage more women to seek help and share their experiences.
- Empowerment: Conversations about sexual desire can empower women to take control of their own bodies and challenge off-putting stereotypes.
- Community Support: Sharing successful treatment stories contributes to a more supportive environment where women are encouraged to explore all available options.
Ultimately, these social and cultural considerations form an essential backdrop to the implementation of clinical guidelines. By addressing these issues head-on, providers and patients together can build a more inclusive and empathetic approach to treatment.
Concluding Thoughts: Embracing a Holistic Future in HSDD Management
The UCSF-led guidelines for low sexual desire in women signal a turning point in the way we address this often misunderstood condition. By integrating medication-based therapies with psychological and lifestyle interventions and by taking a thorough, patient-centered approach, the new recommendations offer a promising blueprint for the future of women’s sexual health.
As providers continue to get around the challenges involved in updating clinical protocols—and as patients gain more confidence in exploring these treatment options—the hope is that no woman will ever again have to suffer in silence due to low sexual desire. Instead, the combined efforts of healthcare professionals and informed patients can foster an environment where every woman’s unique needs are respected and met.
In closing, while the journey to fully implementing these guidelines may be loaded with problems and small distinctions that require careful thought, the long-term benefits for women’s health are clear. The balanced blend of technology, therapy, and tailored care stands as a must-have model for treating HSDD. This model not only paves the way for better health outcomes but also encourages a cultural shift toward more informed and compassionate care in the realm of sexual health.
Final Reflections: A Call for Continued Innovation and Compassion
The emergence of these comprehensive guidelines is a super important moment in modern medicine—a moment that combines the best available evidence with a humane approach to patient care. Whether you are a healthcare provider striving to refine your treatment approach or a patient seeking to understand the options available, these recommendations offer hope and direction. They remind us that even the most complicated pieces of a health issue can be managed with the right mix of expertise, empathy, and innovative thinking.
Let us continue to support research, advocate for better education, and work together to overcome the small twists and turns that come with addressing low sexual desire in women. Future advancements will likely refine these guidelines even further, allowing us to work through the challenges with increasing confidence and compassion. In doing so, we not only improve individual lives but also contribute to a broader movement toward health equity and understanding in the field of sexual medicine.
The road ahead might be full of nerve-racking moments and confusing bits, but with collective effort and a commitment to holistic care, every woman can look forward to living a healthier, more fulfilling life. This is not just a win for modern medicine—it’s a win for all of us who believe that comprehensive, patient-focused care is the key to unlocking true wellbeing.
Originally Post From https://www.ucsf.edu/news/2025/10/430991/first-treatment-guidelines-low-sexual-desire-women
Read more about this topic at
Six lifestyle changes a man can make to improve sexual function
Promoting sexual well-being – PMC – PubMed Central – NIH